| AI in Clinical Medicine, ISSN 0000-0000 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, AI Clin Med and Elmer Press Inc |
| Journal website https://aicm.elmerpub.com |
Review
Volume 1, 2025, e3
Artificial Intelligence in Clinical Medicine: Transforming Diagnosis, Treatment, and Patient Care
Kui Chena, Licun Wub, c, Hong Changd, e
aTranslational Cancer Genomics Program at the Princess Margaret Cancer Centre and the Schwartz Reisman Liver Research Centre, Toronto General Hospital, University Health Network, Toronto, ON, Canada
bLatner Thoracic Surgery Research Laboratories, Division of Thoracic Surgery, Toronto General Hospital, Toronto General Hospital Research Institute, University Health Network, University of Toronto, Toronto, ON M5G 1L7, Canada
cPrincess Margaret Cancer Centre, University Health Network, Toronto, ON M5G 1L7, Canada
dDepartment of Laboratory Hematology, University Health Network, Toronto, Ontario, Canada
eDepartment of Laboratory Medicine and Pathobiology, University of Toronto, Toronto, Ontario, Canada
fCorresponding Author: Licun Wu, Latner Thoracic Surgery Research Laboratories, Division of Thoracic Surgery, Toronto General Hospital, Toronto General Hospital Research Institute, University Health Network, University of Toronto, Toronto, ON M5G 1L7, Canada
Manuscript submitted April 25, 2025, accepted May 5, 2025, published online June 14, 2025
Short title: AI in Clinical Medicine: Revolutionizing Healthcare
doi: https://doi.org/10.14740/aicm3
- Abstract
- Introduction
- The Rise of AI: Human Health Frontier
- AI in Diagnosis: Enhancing Accuracy and Speed
- AI in Treatment: Personalization and Precision Medicine
- AI in Patient Care: Improving Access and Efficiency
- Ethical Considerations and Challenges
- AI Integration for Multimodal and Cross-Domain Clinical Intelligence
- Synergizing AI-Human Expertise for Collaborative Clinical Decision-Making
- The Future of AI in Clinical Medicine
- Conclusion
- References
| Abstract | ▴Top |
Artificial intelligence (AI) is revolutionizing clinical medicine by enhancing diagnostic accuracy, personalizing treatment, and optimizing patient care. In diagnostics, AI-powered systems, such as deep learning models for mammography and dermatology, have demonstrated human-comparable or superior performance, reducing errors and improving early disease detection. In treatment, AI facilitates precision medicine through clinical decision support systems (CDSS) and pharmacogenomics, enabling tailored therapies and accelerating drug discovery. AI also improves patient care via virtual health assistants, remote monitoring, and hospital workflow optimization, increasing accessibility and efficiency. However, challenges such as algorithmic bias, data privacy, transparency, and regulatory hurdles must be addressed to ensure ethical and equitable AI deployment. Future directions include multimodal AI integration, human-AI collaboration, and expanding global health applications to bridge healthcare disparities. As AI continues to evolve, its responsible implementation will be critical in shaping a more predictive, personalized, and inclusive healthcare paradigm.
Keywords: Artificial intelligence; Clinical medicine; Precision medicine; Diagnostic accuracy; Ethical challenges
| Introduction | ▴Top |
Artificial intelligence (AI) is rapidly reshaping the landscape of clinical medicine, ushering in a new era of data-driven decision-making and personalized healthcare. AI technologies, particularly those based on machine learning and deep learning, are being deployed across various domains, from early disease diagnosis to individualized treatment planning and streamlined patient care delivery. For instance, AI has demonstrated human-comparable accuracy in interpreting medical imaging, as seen in Google’s breast cancer detection model, which outperformed radiologists in reducing false positives and negatives [1].
Moreover, AI is accelerating progress in precision medicine by analyzing complex genomic, clinical, and lifestyle data to tailor treatments for individual patients [2]. In hospital settings, AI-driven systems are optimizing workflows, predicting patient deterioration, and improving resource allocation [3]. Crucially, AI is not intended to replace clinicians but to augment their decision-making by providing rapid, evidence-based insights.
As healthcare systems worldwide face growing demands for efficiency, accuracy, and accessibility, AI offers a transformative solution. However, responsible implementation, ensuring transparency, fairness, and clinical validation, remains essential to realizing AI’s full potential in medicine. This article explores AI’s evolving role in diagnosis, treatment, and patient management, while addressing key challenges and future directions in this dynamic field [4, 5].
To frame the evolving relationship between AI and human expertise in clinical medicine, we present a conceptual model illustrating their complementary roles across eight interconnected domains, including diagnosis, treatment, patient care, ethics, data integration, and innovation. As shown in Figure 1, this framework highlights how human-AI collaboration can reshape modern healthcare through synergy rather than separation.
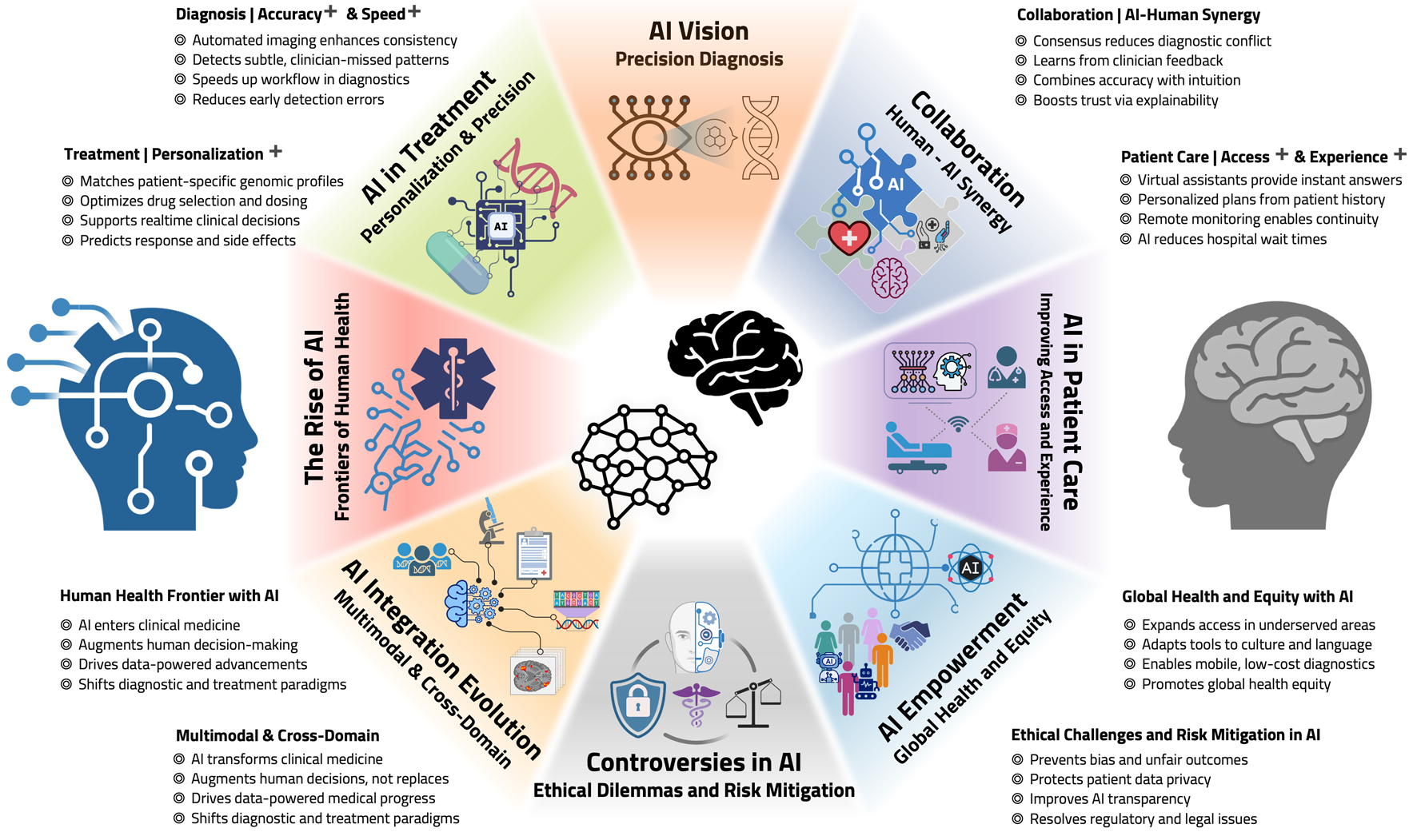 Click for large image | Figure 1. A conceptual model of human-AI integration in clinical medicine. This diagram presents a conceptual framework for understanding the complementary roles of AI and human expertise in clinical medicine. AI contributes speed, computational power, precision, and scalability, while human clinicians offer empathy, contextual insight, intuitive reasoning, and ethical judgment. Surrounding this core are eight key domains that reflect the multifaceted integration of AI into clinical workflows, including diagnosis, treatment, patient care, equity, ethics, collaboration, data integration, and global health. This model emphasizes that meaningful innovation in medicine emerges from collaboration, not replacement, between humans and machines. Some elements in this figure, including specific icons and biological illustrations, were created using BioRender (BioRender.com). AI: artificial intelligence. |
| The Rise of AI: Human Health Frontier | ▴Top |
AI is entering clinical medicine as a transformative force, not to replace human expertise but to enhance and complement it. Unlike past technologies that merely automated tasks, AI introduces a new paradigm: one where computational reasoning and human clinical judgment coexist symbiotically. Rather than viewing AI as a disruptive threat, this chapter frames its emergence as the beginning of a new era of collaborative intelligence.
By weaving together pattern recognition, probabilistic inference, and real-time learning, AI redefines how we think about diagnosis, treatment, and decision-making. This evolving partnership between AI and clinicians forms the conceptual backbone of this review, inviting a reimagining of medicine rooted in balance, mutual augmentation, and trust.
| AI in Diagnosis: Enhancing Accuracy and Speed | ▴Top |
Among the most transformative applications of AI in clinical medicine is its role in disease diagnosis. AI systems can rapidly process and analyze massive datasets from electronic health records (EHRs), medical imaging, histopathology, and genomic sequences to identify patterns that may elude even experienced clinicians. This results in earlier detection, more accurate diagnoses, and improved patient outcomes.
Radiology and medical imaging
In radiology, deep learning models, especially convolutional neural networks (CNNs), have shown remarkable performance in interpreting medical images. A landmark study by McKinney et al (2020) demonstrated that a deep learning system developed by Google Health could detect breast cancer in mammograms with an accuracy comparable to, or even better than, expert radiologists. The AI reduced both false positives and false negatives, showing potential for augmenting radiologist workflows and reducing diagnostic burden in high-volume settings [1].
Similarly, in dermatology, AI systems have achieved dermatologist-level accuracy in classifying skin lesions. Esteva et al (2017) trained a CNN on over 129,000 clinical images and demonstrated that the model could distinguish between malignant and benign lesions as accurately as board-certified dermatologists, making it particularly valuable in underserved regions with limited specialist access [6].
Pathology and laboratory medicine
AI is revolutionizing pathology by digitizing and analyzing histopathological slides. Companies like PathAI use machine learning to detect cancerous cells with improved precision, reducing inter-observer variability and diagnostic errors. Litjens et al (2017) provided a comprehensive overview of how deep learning models can aid in detecting metastases in breast cancer pathology slides with high sensitivity, helping pathologists make faster and more reliable decisions [7].
In sum, AI enables faster, more consistent, and scalable diagnostic processes across multiple specialties, promising a new era of precision diagnostics in medicine.
| AI in Treatment: Personalization and Precision Medicine | ▴Top |
AI is playing an increasingly critical role in the evolution of personalized medicine, empowering clinicians to tailor treatment plans to individual patients based on complex datasets. By integrating genomic information, clinical records, and real-time patient data, AI facilitates more precise, effective, and safer treatments.
Clinical decision support systems (CDSS)
AI-powered CDSS are helping physicians make informed, data-driven decisions. These tools can analyze vast amounts of patient data, including lab results, imaging, genomics, and clinical guidelines, to suggest treatment options or flag adverse drug interactions. A notable example is IBM Watson for Oncology, which uses natural language processing and machine learning to synthesize data from thousands of sources, including peer-reviewed articles and patient histories, to generate cancer treatment recommendations. Chen et al (2019) found that Watson’s treatment suggestions aligned with oncologist decisions in a majority of breast cancer cases in China, illustrating its potential as a second opinion tool [8].
Pharmacogenomics and drug development
AI is also transforming pharmacogenomics, where it helps predict how patients will respond to specific medications based on their genetic makeup. This leads to more effective treatments and fewer adverse drug reactions. Additionally, AI is accelerating drug discovery and development by predicting drug-target interactions, optimizing compound screening, and simulating clinical trial outcomes. A major breakthrough in this area is DeepMind’s AlphaFold2, which solved the decades-old challenge of predicting protein structures with remarkable accuracy. This advancement, described by Jumper et al (2021), is poised to dramatically speed up drug discovery and reduce associated costs [2].
In essence, AI enables a shift from one-size-fits-all therapies to personalized treatment strategies, improving outcomes and laying the foundation for a more predictive, preventative, and participatory healthcare model.
| AI in Patient Care: Improving Access and Efficiency | ▴Top |
Beyond transforming diagnosis and treatment, AI is significantly improving the delivery of patient care by enhancing efficiency, accessibility, and patient engagement. These innovations help to bridge resource gaps, reduce clinician workload, and empower patients in managing their health.
Virtual health assistants and chatbots
AI-powered chatbots and virtual assistants, such as Babylon Health, Ada Health, and Buoy, are reshaping how patients interact with healthcare systems. These platforms provide 24/7 access to health information, conduct symptom triage, assist with appointment scheduling, and offer medication reminders. For instance, Bickmore et al (2018) demonstrated that conversational agents can improve patient engagement and adherence to treatment plans, especially in managing chronic conditions [9]. In telemedicine and primary care, these tools relieve pressure on clinicians and reduce unnecessary visits, allowing healthcare systems to focus resources where they are most needed.
Remote monitoring and predictive analytics
AI integrated with wearable technologies allows for real-time health monitoring outside of traditional clinical settings. Devices like Apple Watch and KardiaMobile use AI algorithms to detect atrial fibrillation, flagging abnormalities for early intervention. A study by Tison et al (2018) showed that deep learning applied to smartwatch electrocardiogram (ECG) data could detect atrial fibrillation with high accuracy, improving preventive care for at-risk populations [10].
Hospital workflow optimization
Healthcare systems also leverage AI to improve operational efficiency. Tools for predicting hospital admissions, optimizing staffing schedules, and managing supply chains are being adopted to reduce wait times, lower operational costs, and improve patient throughput. Rajkomar et al (2019) emphasized that machine learning models trained on EHR data could forecast patient demand and optimize resource allocation, contributing to a smoother clinical workflow [3].
| Ethical Considerations and Challenges | ▴Top |
While the integration of AI into clinical medicine holds tremendous promise, it also brings forth a complex array of ethical, legal, and technical challenges that must be thoughtfully addressed to ensure safe, equitable, and responsible implementation.
Bias and fairness
One of the most pressing concerns is the risk of algorithmic bias. AI systems are only as good as the data they are trained on. If training datasets reflect existing social and healthcare inequalities, the AI can unintentionally reinforce those disparities. For example, Obermeyer et al (2019) revealed that a widely used healthcare algorithm underestimated the health needs of Black patients because it used healthcare costs as a proxy for health status, leading to biased treatment recommendations [11]. Addressing such issues requires greater diversity in training data and deliberate fairness auditing of algorithms.
Data privacy
The use of large-scale patient data raises critical privacy and security concerns. AI models often rely on extensive datasets drawn from EHRs, imaging databases, and genomics. Ensuring compliance with data protection regulations like HIPAA (in the USA) and GDPR (in the EU) is essential to maintain patient confidentiality and trust [12].
Transparency and explainability
Many high-performing AI systems, especially those based on deep learning, operate as “black boxes”, providing results without clear explanations. This lack of transparency can hinder clinician trust and impede clinical decision-making, especially when errors occur [13].
Regulatory hurdles
AI-driven tools often evolve rapidly and continuously learn from new data. Traditional regulatory pathways are not well-suited for such dynamic systems. Regulatory agencies like the FDA are working to adapt, including proposing a framework for a “total product lifecycle” approach to AI in medicine [14]. However, harmonizing international regulations remains a challenge.
| AI Integration for Multimodal and Cross-Domain Clinical Intelligence | ▴Top |
AI is uniquely capable of integrating diverse medical data streams, such as imaging, EHRs, and next-generation sequencing (NGS), into unified analytical models. This multimodal fusion enables AI to reveal relationships that are difficult to discern within siloed datasets, supporting more nuanced clinical insights.
Unlike traditional systems, AI handles noisy, incomplete, and heterogeneous inputs using probabilistic and attention-based architectures. This adaptability allows models to operate effectively in real-world scenarios where missing data, inconsistent formats, or fragmented medical histories are common.
Crucially, AI enables cross-domain reasoning, for example, linking radiologic tumor patterns with genomic mutations and EHR-documented symptoms, to suggest more tailored treatment decisions. This convergence of modalities facilitates comprehensive patient profiling that supports personalized care and population-level learning simultaneously.
| Synergizing AI-Human Expertise for Collaborative Clinical Decision-Making | ▴Top |
AI augments, not replaces, clinician judgment. In modern healthcare, synergy between human expertise and machine intelligence enables more accurate, consistent, and explainable decision-making. Consensus modeling blends AI’s pattern recognition with clinician input to reduce inter-observer variability, especially in ambiguous or high-stakes diagnoses. Human-in-the-loop learning allows AI systems to evolve through expert feedback, improving over time based on clinical corrections. This collaboration balances computational precision with human intuition, combining data-driven analysis with contextual understanding. Explainable AI (XAI) tools, such as attention maps or interpretable outputs, build clinician trust, making AI a transparent and accountable partner in care delivery.
| The Future of AI in Clinical Medicine | ▴Top |
Multimodal AI
A major frontier in AI-driven healthcare is the development of multimodal AI systems, which integrate diverse data sources, such as medical imaging, EHRs, genomic data, laboratory results, and patient-reported outcomes, into cohesive analytical frameworks. These systems offer more comprehensive and accurate health assessments by bridging traditionally isolated data streams. For instance, the MARIA model (Multimodal Attention Resilient to Incomplete datA) introduced in late 2024 employs a transformer-based architecture to effectively handle incomplete multimodal healthcare data, enhancing predictive performance even when certain data modalities are missing [15]. Similarly, the M3H framework (Multimodal Multitask Machine Learning for Healthcare) presented at NeurIPS 2024 demonstrates an explainable approach that consolidates learning from various data types, including tabular, time-series, language, and vision data, for multiple tasks such as classification, regression, and clustering. As AI technologies continue to advance, these multimodal systems are expected to revolutionize clinical workflows, improve diagnostic precision, and foster greater patient engagement by integrating more seamlessly into everyday medical practice [16].
Human-AI collaboration
A key advancement in AI-driven healthcare is the integration of human-AI collaboration, where AI systems augment, rather than replace, clinicians’ decision-making processes. Recent studies demonstrate that combining physician expertise with AI enhances diagnostic accuracy beyond what either can achieve independently. For instance, Awasthi et al (2024) introduced CoRaX, a collaborative AI system that integrates eye gaze data and radiology reports to identify and correct perceptual errors in chest radiographs. In a study involving 271 samples with 28% missed abnormalities, CoRaX corrected 21% of these errors, demonstrating its efficacy in enhancing radiological diagnostics [17].
Similarly, Strong et al (2024) developed a guided deferral system leveraging large language models (LLMs) to intelligently defer uncertain cases to human clinicians. This approach mitigates the risk of AI-generated inaccuracies by combining AI’s computational strengths with human judgment, leading to improved decision-making in clinical settings [18].
These advancements underscore the transformative potential of human-AI collaboration in healthcare, enhancing diagnostic precision and patient outcomes through synergistic integration of technology and human expertise.
Global health applications
AI tools are increasingly pivotal in bridging gaps in medical expertise and resources, especially in underserved regions. Their application in global health is transforming access to quality care by providing clinical decision support in low-resource settings where specialists are scarce. For instance, the AI Clinics on Mobile (AICOM) project, introduced in 2023, enables AI-based disease diagnostics and screening on affordable mobile phones without requiring internet connectivity. This approach has been demonstrated effective in tasks like monkeypox screening, aiming to evolve into a universal AI doctor for underserved and hard-to-reach populations [19].
Similarly, a 2025 study developed an AI-enabled smartphone application for real-time fetal assessment in rural Guatemala. This tool assists midwives during home visits by providing immediate analysis and feedback, enhancing maternal and neonatal health outcomes in areas with limited healthcare infrastructure [20].
These advancements underscore the transformative potential of AI in democratizing healthcare access and reducing disparities in underserved regions.
In summary, the future of AI in clinical medicine is not solely about automation but about enhancing the precision, equity, and reach of healthcare. By leveraging multimodal data, fostering collaborative intelligence, and addressing global disparities, AI promises to reshape medicine into a more predictive, personalized, and inclusive discipline.
| Conclusion | ▴Top |
AI is not a distant vision but a present-day reality in clinical medicine. From augmenting diagnostic accuracy to personalizing treatments and improving patient care logistics, its impact is profound and far-reaching. However, realizing AI’s full potential will require interdisciplinary collaboration, robust ethical frameworks, and continuous evaluation to ensure it serves all patients equitably and safely.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Author Contributions
Licun Wu, Kui Chen, and Hong Chang jointly conceived the research idea and designed the study. Licun Wu wrote the original draft of the manuscript, while Hong Chang critically reviewed, edited, and finalized the manuscript. Kui Chen developed the diagram to visually summarize the core concept of this work.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- McKinney SM, Sieniek M, Godbole V, Godwin J, Antropova N, Ashrafian H, Back T, et al. International evaluation of an AI system for breast cancer screening. Nature. 2020;577(7788):89-94.
doi pubmed - Jumper J, Evans R, Pritzel A, Green T, Figurnov M, Ronneberger O, Tunyasuvunakool K, et al. Highly accurate protein structure prediction with AlphaFold. Nature. 2021;596(7873):583-589.
doi pubmed - Rajkomar A, Dean J, Kohane I. Machine learning in medicine. N Engl J Med. 2019;380(14):1347-1358.
doi pubmed - https://chat.deepseek.com/.
- https://chatgpt.com/.
- Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, Thrun S. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115-118.
doi pubmed - Litjens G, Sanchez CI, Timofeeva N, et al. Deep learning as a tool for increased accuracy and efficiency of histopathological diagnosis. Medical Image Analysis. 2017;42:103-111.
doi - Chen M, Hao Y, Cai Y, et al. The application of Watson for Oncology in breast cancer treatment recommendations in China. Journal of Clinical Oncology. 2019;37(15_suppl):e13523.
doi - Bickmore TW, Trinh H, Olafsson S, O'Leary TK, Asadi R, Rickles NM. Patient and consumer safety risks when using conversational assistants for medical information: An observational study of Siri, Alexa, and Google Assistant. Journal of Medical Internet Research. 2018;20(9):e10163.
doi - Tison GH, Sanchez JM, Ballinger B, Singh A, Olgin JE, Pletcher MJ, Vittinghoff E, et al. Passive detection of atrial fibrillation using a commercially available smartwatch. JAMA Cardiol. 2018;3(5):409-416.
doi pubmed - Obermeyer Z, Powers B, Vogeli C, Mullainathan S. Dissecting racial bias in an algorithm used to manage the health of populations. Science. 2019;366(6464):447-453.
doi pubmed - Price WN, 2nd, Cohen IG. Privacy in the age of medical big data. Nat Med. 2019;25(1):37-43.
doi pubmed - Samek W, Wiegand T, Muller KR. Explainable Artificial Intelligence: Understanding, visualizing and interpreting deep learning models. In: Digital Signal Processing. Springer. 2017;73:1-15.
doi - U.S. Food & Drug Administration (FDA). Proposed regulatory framework for modifications to artificial intelligence/machine learning (AI/ML)-based software as a medical device (SaMD). 2019. https://www.fda.gov/media/122535/download.
- Caruso CM, Soda P, Guarrasi V. MARIA: a multimodal transformer model for incomplete healthcare data. arXiv preprint. 2024.
- Bertsimas D, Ma Y. M3H: multimodal multitask machine learning for healthcare. Presented at NeurIPS 2024 Workshop on Advancements In Medical Foundation Models. 2024.
- Awasthi A, Le N, Deng Z, Wu CC, Nguyen HV. Enhancing radiological diagnosis: a collaborative approach integrating AI and human expertise for visual miss correction. arXiv preprint. 2024.
- Strong J, Men Q, Noble A. Towards human-AI collaboration in healthcare: guided deferral systems with large language models. arXiv preprint. 2024.
- Chowdhury MEH, Khandakar A, Abdur Rahman T, et al. AI clinics on mobile (AICOM): an offline AI-powered medical diagnostic system for low-resource settings. arXiv preprint. 2023.
doi - Reyes AM, Rios DC, Samayoa AS, et al. Smartphone-based AI for real-time fetal health assessment in rural Guatemala. arXiv preprint. 2025.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
AI in Clinical Medicine is published by Elmer Press Inc.